Understanding the health effects and susceptibility factors of circadian misalignment – Publicly Invited Research 2016-2017
- A02 Shinohara
- A02 Maekawa
- A02 Ohgami
- A02 Nishimura
- A02 Kawano
- A02 Iwase
- A02 Furuichi
- A02 Myung
- A02 Kitamura
| Research Subject | Understanding the health effects and susceptibility factors of circadian misalignment |
|---|---|
| Research Group Leader |

|
| Research Collaborator(s) |
|
Objectives
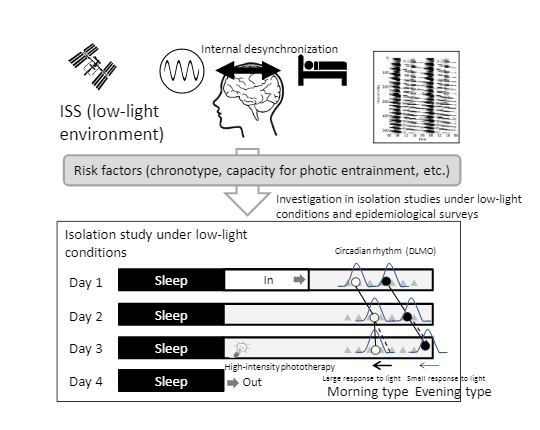
Under low-light conditions in the isolated environment of the International Space Station (ISS), maintaining a proper relationship between the sleep-wake cycle and biological rhythms is difficult, even with adequate sleep time, and likely contributes to internal desynchronization. Recent studies have shown that internal desynchronization of just 1 h due to a busy social schedule—a condition known as social jet lag—has detrimental effects on mental and physical well-being. However, the risk factors for internal desynchronization have not been fully investigated to date.
In addition to epidemiological surveys, we conduct isolation experiments by simulating the lighting environment of the ISS to investigate the development of internal desynchronization in low-light environments. We also investigate the risk factors for internal desynchronization (chronotypes, capacity for photic entrainment, and other social and biological factors).
Summary of previous findings
1. Risk of developing circadian rhythm sleep disorder due to a prolonged intrinsic circadian period
Circadian rhythm sleep disorder free-running type, a sleep disorder characterized by a daily delay of about 1 h in the sleep-wake cycle, causes serious problems in social life due to periodic nocturnal insomnia, daytime sleepiness, and comorbid mental disorders. In a study using a forced desynchronization protocol, we carefully investigated the effect of the special sleep schedule on the biological clock in 6 patients with circadian rhythm sleep disorder free-running type and 17 healthy individuals with intermediate or evening chronotype. We found that the period (τ) was 24.48 ± 0.05 h in patients, which was much longer than 24.12 ± 0.07 h observed in intermediate chronotypes. This suggests that patients with circadian rhythm sleep disorder free-running type have difficulty entraining the biological clock to the 24-h light-dark cycle. However, τ of patients partially overlapped τ of healthy individuals with evening chronotypes (24.22 ± 0.10 h), suggesting the involvement of multiple factors, such as the capacity for photic entrainment.
2. Evening chronotype as a risk factor for depression
To determine the relationship between evening preference and depression, we investigated chronotype (morning or evening type), sleep conditions, and the prevalence of depression in 1,170 adult men and women (mean age of 38.5 years). The results showed that individuals with a strong evening preference tended to have a delayed sleep phase, short sleep duration, poor subjective sleep quality, strong daytime sleepiness, and a high prevalence of depression. Logistic regression analysis showed a significant positive correlation between strong evening preference and depression, independent of sleep duration or sleep quality.
3. Validity of the Japanese version of the Munich Chronotype Questionnaire
The Munich Chronotype Questionnaire (MCTQ) is a useful tool for determining individuals’ chronotypes from their sleep patterns for a day with no work-, school-, or housekeeping-related constraints. We conducted the MCTQ survey with 450 community-dwelling residents and found a significant correlation between the MCTQ and the standard Morningness-Eveningness Questionnaire (MEQ). Furthermore, in a study with 37 adult men and women, we found that the onset of melatonin secretion correlated more strongly with the MCTQ than with the MEQ. These findings verify the utility and validity of the Japanese version of the MCTQ.
Research plan for this fiscal year
To elucidate the development of internal desynchronization in low-light environments, we will simulate the lighting environment of the ISS (around 150 lux during a wake period) in a 4-day isolation study of healthy adults with different chronotypes. The onset of internal desynchronization will be evaluated using the dissociation between a circadian rhythm phase (onset of melatonin secretion) and a sleep-wake cycle as an indicator. Subjects will stay in a laboratory under dim daytime lighting conditions (approximately 150 lux) and then be exposed to a high-intensity phototherapy device for 1 h on the morning of Day 3. The contribution of chronotype and the capacity for photic entrainment to the development of internal desynchronization will be investigated.